Abstract
BACKGROUND: Production of chimeric antigen receptor (CAR) -engineered T cells is currently done for each patient individually and relies on a patient-derived T cell product of heterogeneous quality. On target/off tumor effects represent a major obstacle for a broader application of CARs. Broader application of this powerful therapeutic tool is hampered by limited production capacity and the non-desired sequelae from CAR-derived on target/off tumor effects. Here we investigated whether precursor T cells (preTs) engineered to express a clinically relevant CAR can potentially address some of these limitations.
METHODS: Murine LSK cells were transduced with a 2nd generation murine CAR (CD28CD3zeta configuration) against CD19 in a lentiviral backbone and consecutively differentiated into preTs using the OP9-DL1 feeder layer system. CAR-engineered preTs (8 x 106) of MHC matched (B6/NCrl) or mismatched origin (B10.A) were co-transplanted with syngeneic T-cell-depleted bone marrow into irradiated B6 recipients. Mice were challenged with a lethal dose of CD19+ murine leukemia cells 20 days after adoptive transfer and assessed for B cell recovery and survival. For in vivo NK cell depletion studies, the anti-NK1.1 antibody (clone: PK136) was used. Sorted CAR preTs previous to co-transfer and after in vivo maturation were analyzed by microarray technology.
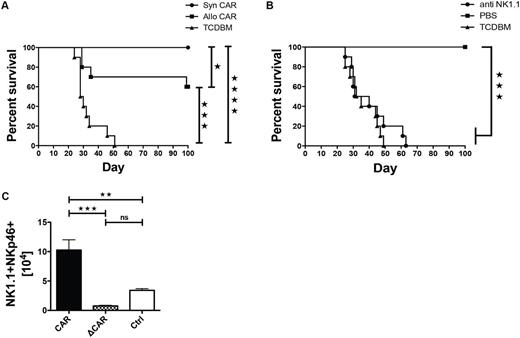
RESULTS: Afterco-transplantation of in vitro generated CAR-engineered preTs up to 60% (p<0.001) and 100% (p<0.0001) leukemia free survival was achieved in fully MHC-mismatched or MHC-matched recipients respectively (Figure 1A). No graft-versus-host disease was induced. Anti-leukemic effects entirely relied on the in vivo development of CAR-expressing natural killer (NK) cells since NK cell depletion after hematopoietic stem cell transplantation (HCT) resulted in a complete abrogation of anti-leukemic effects (Figure 1B, p<0.001). As shown by gene expressing profiling enforced CAR-expression on preTs fosters transcriptional key factors being associated with NK cell development such as Nfil3, Id2, and Eomes. CAR-expression on co-transplanted preTs blocked thymic seeding completely and prevented further T-cell development in vivo. In contrast, CAR-expression favored NK cell development with strong anti-leukemic effects when compared to signaling-defective CAR preTs early after adoptive transfer of engineered preTs (Figure 1C, p<0.001). CAR-bearing NK-cells persisted for up to 60 days post-transplant allowing for complete B-cell recovery thereafter.
CONCLUSION: Co-transplantation of CAR-engineered preTs is of high clinical relevance since they can be prefabricated and frozen as a "off the shelf product". Limited persistence of their NK-progenies after HCT makes them an attractive platform for CARs when on target/off tumor effects are of specific concern.
Figure 1: Co-transplantation of mCD19 CAR-engineered preTs provides strong anti-leukemia effects that are mediated by preT-derived CAR-expressing NK cells. (A) Irradiated B6/NCrl recipients were transplanted with either 3 x 106 T cell depleted bone marrow cells (TCDBM) only (n= 10) or additionally with 8 x 106 of either syngeneic (n= 10) or allogeneic CAR-transduced preTs (n= 10). Mice were challenged with 1.2 x 106 C1498-CD19-GFP cells on day 20 after transplantation (day 0) and followed for survival (B) Mice co-transplanted with CAR-preTs were treated i.p. weekly either with a depleting anti-NK1.1 antibody (200µg) or with PBS for control (n= 10, respectively). All mice received 1.2 x 106 C1498-CD19-GFP cells on day 20 after transplantation and survival was assessed after leukemia challenge. (C) Progenies of co-transplanted CAR-, ΔCAR- (CAR defective for signaling) or Ctrl-transduced preTs were analyzed within the BM of transplanted mice by flow cytometry 14 days after transplantation. Numbers of NK1.1+NKp46+ cells within the gate are depicted (CAR, ΔCAR, Ctrl, n=4 respectively). (A, B) Survival curves were analyzed with Mantel-Cox (log-rank) test and (C) with one-way ANOVA followed by Turkey`s post-test. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Sauer: Neovii: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.